Colorectal cancer affects the colon or rectum, two interconnected parts of the large intestine that play a significant role in the digestive process. This is the third most commonly diagnosed cancer in the United States. Here is more information on this type of cancer, its risk factors, and how it’s detected:
Exploring Colorectal Cancer
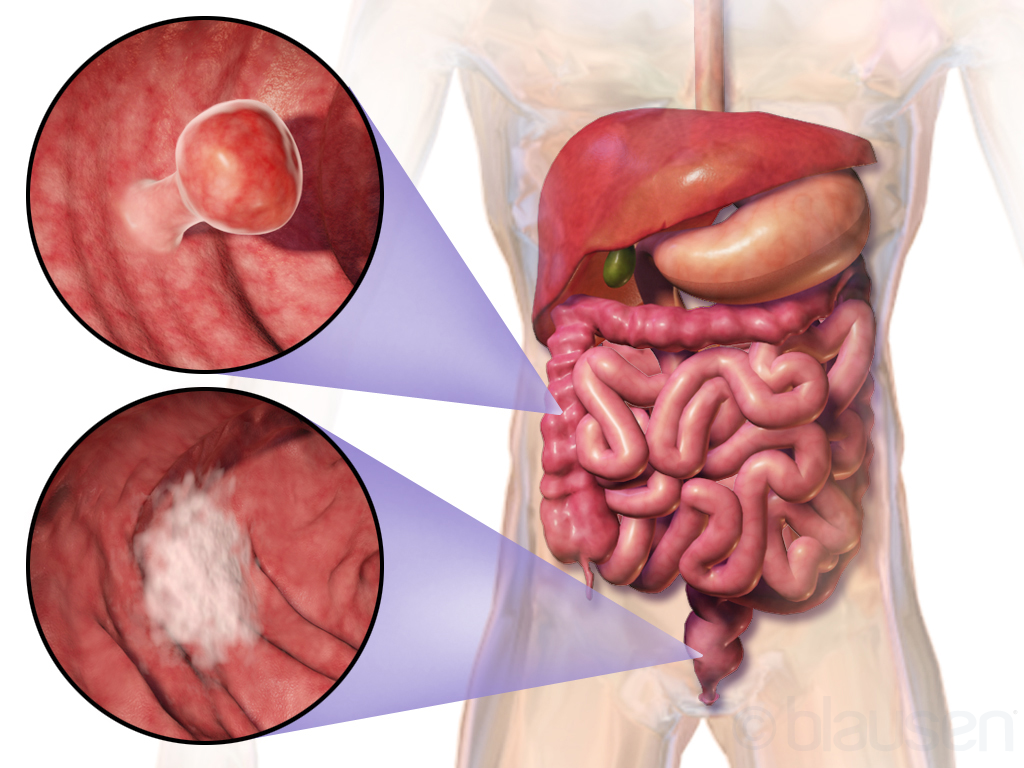
Colorectal cancer develops when cells in the colon or rectum begin growing abnormally and form tumors. The colon, also known as the large intestine, connects to the rectum, which serves as the final section before waste exits the body. Cancer can occur anywhere along this pathway, with different locations sometimes presenting distinct characteristics.
Most colorectal type cancers begin as small, benign growths called polyps that develop on the inner lining of the colon or rectum. These polyps typically remain harmless for years, but some types can gradually transform into cancerous tissue over time. The transformation process usually occurs slowly, often taking 10 to 15 years for normal cells to become cancerous.
Different types of polyps carry varying levels of risk. Adenomatous polyps represent the most common precancerous type, while hyperplastic polyps typically pose minimal risk. The size, number, and specific characteristics of polyps influence their potential for becoming cancerous. Healthcare professionals classify cancer into several stages based on how far the cancer has spread beyond its original location.
Identifying Risk Factors
Age is the most significant risk factor for colorectal cancer, with most cases occurring in people over 50 years old. The incidence increases steadily with age, making regular screening particularly relevant for older adults. Recent data show that rates among younger adults have been rising. Family history and genetic factors play a substantial role in cancer risk. Individuals with close relatives who have had colorectal cancer face an increased risk, especially if the relative developed cancer before age 50. Specific genetic conditions, such as Lynch syndrome and familial adenomatous polyposis, significantly elevate risk levels.
Lifestyle factors contribute to cancer development in various ways. Diets high in red meat and processed foods may increase risk, while diets rich in fruits, vegetables, and whole grains may provide protective benefits. Physical inactivity, obesity, smoking, and excessive alcohol consumption all contribute to elevated risk levels.
Understanding Detection Methods
Colorectal cancer symptoms often develop gradually and may not appear until the disease has progressed. Changes in bowel habits, including persistent diarrhea or constipation, represent common early indicators. Blood in stool, either visible or detected through testing, frequently prompts medical evaluation. Abdominal symptoms include cramping, pain, or discomfort that persists for more than a few days. Unexplained weight loss, fatigue, and weakness can indicate advanced disease. Some individuals experience a feeling of incomplete bowel emptying or rectal bleeding that warrants medical attention.
Detection methods include various screening tests that can identify cancer or precancerous polyps before symptoms develop. Colonoscopy remains the gold standard screening method, allowing direct visualization of the entire colon and rectum. This procedure enables healthcare professionals to detect and remove polyps during the same session.
Learn More About Colorectal Cancer
Colorectal cancer develops in the colon or rectum, typically beginning as benign polyps that can transform into cancerous tissue over many years. Age represents the primary risk factor, though family history, lifestyle choices, and certain medical conditions also influence development. If you’re experiencing any of these symptoms, consult with a gastroenterologist to see if you are at risk.
- HMS Photovoltaik: A Complete, In-Depth Guide to Modern Solar Power Solutions
- Decreto Supremo 160: A Complete and Updated Guide
- Dentiloquent: A Complete Professional Guide
- Närkes Elektriska: Your Trusted Partner in Electrical Services in Örebro, Sweden
- Litorotica Tags: Guide for Better Search, Safety, and Clarity